The Latest
View all
Should I be worried if my daughter’s first period is early?
It’s a fact that over the last few centuries the age of puberty onset has dropped significantly. But how early is too early? When you had your first period, were you concerned that it came too early or too late?
Periods
View allSexual Health
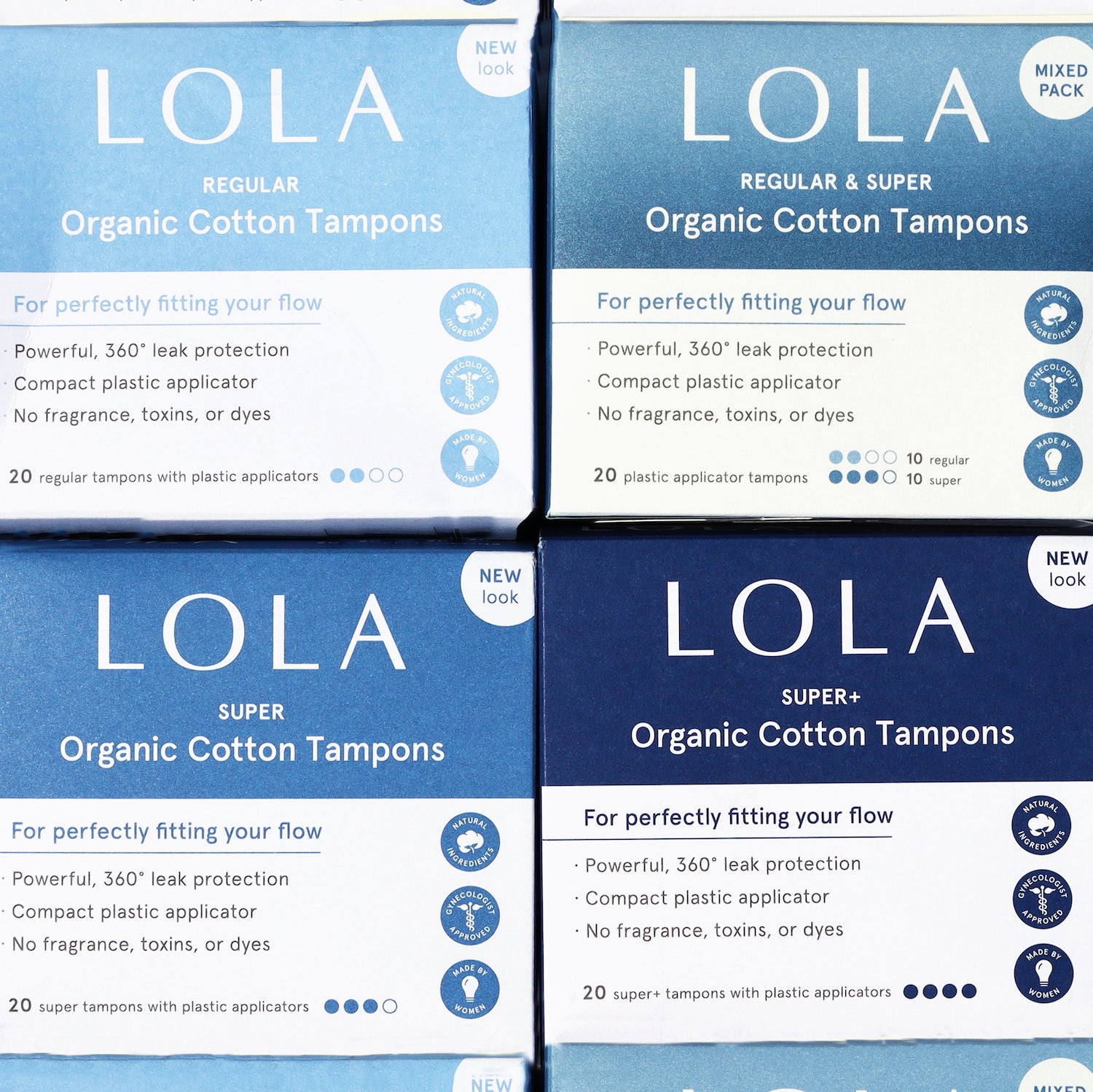
View allShop Best Sellers
View all-
Customizable
-
-
-
Not to cramp your style...
For orders over $400, please purchase from our B2B Website.
SHOP B2B